By Gretchen Hammer
The experience of military service can have a profound impact on a veterans life. I have listened as the veterans in my family recount with pride their service to our great country and with pain some of the difficult experiences of combat.
The sacrifices they and our family made are real, and a real testament to their commitment to our country. As we come together to celebrate Veterans Day it is important that we consider how we might repay this commitment with a promise of our own: The promise of access to high-quality, affordable health care.
Understanding the health and particularly mental health needs of our Colorado veterans is the first step toward doing that. One in eight Coloradans is a veteran. In general, veterans in Colorado have higher average incomes, have higher levels of educational attainment and are more likely to have health insurance than non-veterans.
However, many veterans are in worse health than members of the general population. A recent analysis of national data, estimates over 16 percent of all veterans report having limitations in their health such as trouble getting around and living independently, or problems with their vision or hearing.
Nationally veterans have twice the rate of suicide than the general population. In Colorado, the number is even more troubling. The suicide rate for Colorado veterans is 41.8 deaths per 100,000 people, nearly three times the suicide rate for the general population in Colorado.
Many people erroneously believe that all veterans are eligible for health care through the Veterans Administration system. In fact, access to Veterans Administration benefits is based on a priority system and the nature of discharge from military services, length of services, service related disabilities, income and available VA resources.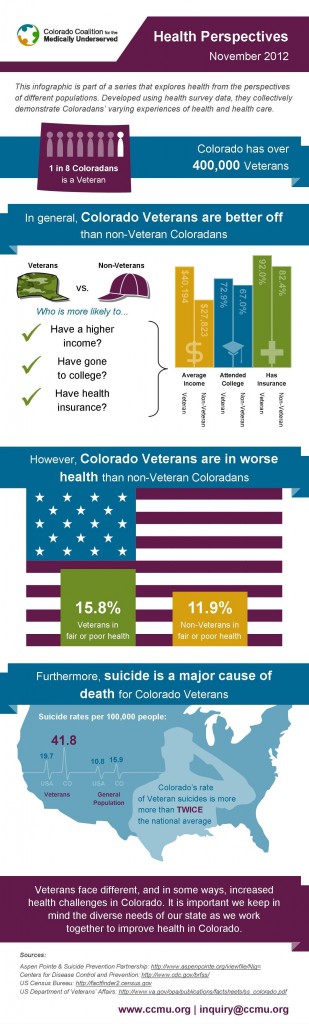
Some veterans have options depending on their needs. Older veterans or veterans with certain disabilities are eligible for Medicare and can choose to enroll in Medicare only, VA benefits only or both. Many veterans, however, are uninsured. It is estimated there are approximately 24,000 uninsured veterans and an additional 17,000 family members that are uninsured in Colorado. One-third of these family members are children.
To address the growing health care needs of our veterans, communities across Colorado are starting to pursue innovative solutions. The Department of Veterans Affairs has invested $580.2 million to build the new Denver VA Medical Center facility on the University of Colorados Anschutz Medical Campus. The Mental Health Center of Denver and the VA have developed a new partnership to speed up the evaluation of post-combat veterans with possible Post-Traumatic Stress Disorder and Traumatic Brain Injury. Pikes Peak Hospice & Palliative Care participates in We Honor Veterans, a pioneering campaign developed by National Hospice and Palliative Care Organization in collaboration with the Department of Veterans Affairs.
Action that we can take at the state level to improve access to health insurance for veterans is to continue to grow and strengthen Medicaid as allowed under federal law.
Nationally, 49 percent of uninsured veterans and 36 percent of uninsured family members of veterans have incomes that would likely enable them to qualify for Medicaid if it is made available. If we apply these national percentages to our uninsured veterans and family member estimates, we could create the opportunity for nearly 18,000 veterans and family members of veterans to enroll in Medicaid.
In addition, many veterans may find new options for purchasing coverage for themselves and their families through the Colorado Health Benefit Exchange. Depending on their income and the availability of other coverage, many veterans and their families may qualify for premium subsidies to make the coverage they buy through the exchange more affordable.
The promise of access to high-quality, affordable health care is one we can deliver on for our veterans if we continue to work together in communities to understand and address the health needs of veterans and their families and if we pursue all avenues to increase health insurance options for veterans who are currently without adequate health coverage.
Gretchen Hammer is executive director of the Colorado Coalition for the Medically Underserved.
